A breast cancer diagnosis or known hereditary risk for developing breast cancer can bring many considerations and decisions—including mastectomy. It’s okay to feel overwhelmed, and it’s important to know your options for mastectomy and reconstruction so your care team can create a plan that supports your needs and aligns with your goals for life after treatment.
One sometimes overlooked aspect of mastectomy is its impact on sensory nerves. Many people are caught off guard by a surprising side effect of mastectomy: numbness.1 To better understand why this happens, let’s look at what happens to nerves during a mastectomy and explore options to help regain sensation as part of your treatment plan.
How does breast sensation work?
Sensory nerves run throughout your body, allowing you to feel and interact with your surroundings. These nerves act like an electrical cord that are made of nerve fibers that transmit signals from your body to your brain. They allow you to feel sensations such as a hug, an intimate touch and a warm shower, and keep you safe by helping you feel burns or cuts. Sensory nerves also help you sense where your body is in space, and how it’s moving—like being able to walk without looking at your feet, or instinctively rotating your torso to pass through a narrow doorway. Read more about how nerves work.
There are multiple nerves that supply sensation to your skin, breast and nipple, including three significant branches of the intercostal nerves. These nerves travel from your spine to your chest wall, branching throughout your breast tissue, with the densest collection of nerves in your nipple and areola (Figure 1).2,3
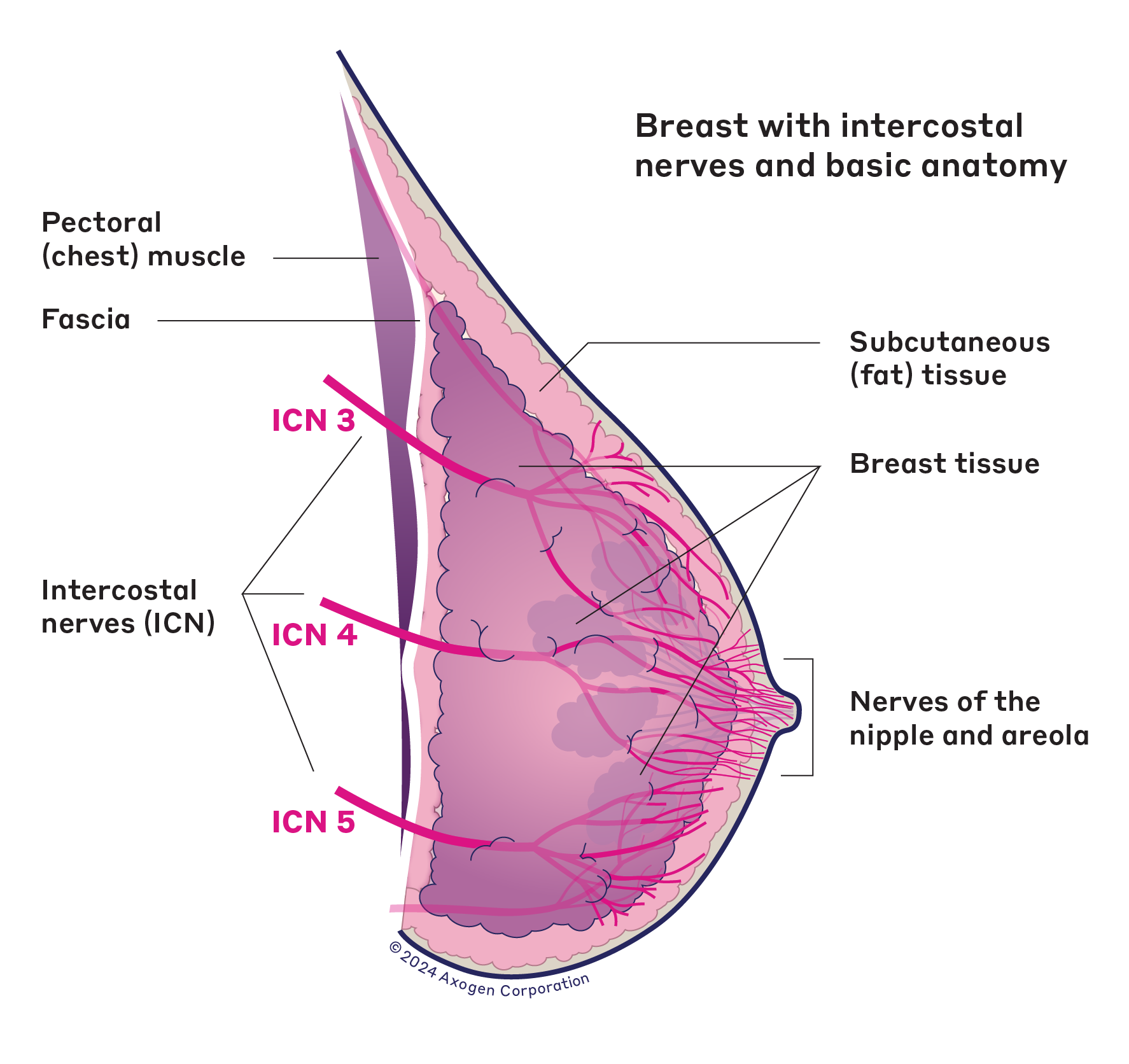
Figure 1: Breast with intercostal nerves and basic anatomy
What happens to nerves during a mastectomy, and how does sensation loss occur?
During a mastectomy, the breast surgeon’s priority is to ensure the safe removal of all breast tissue—cancerous or high-risk (Figure 2). Because nerves typically run throughout the breast tissue, it’s not possible to safely remove the tissue without also removing the nerves within it.2 The placement of the mastectomy incision may vary based on a variety of factors, but it’s unlikely that the location will alter the cutting and removal of breast tissue and nerves. Even in a nipple-sparing mastectomy, breast surgeons generally cannot avoid cutting the nerves that supply sensation to the nipple and areola (Figure 3).2,3
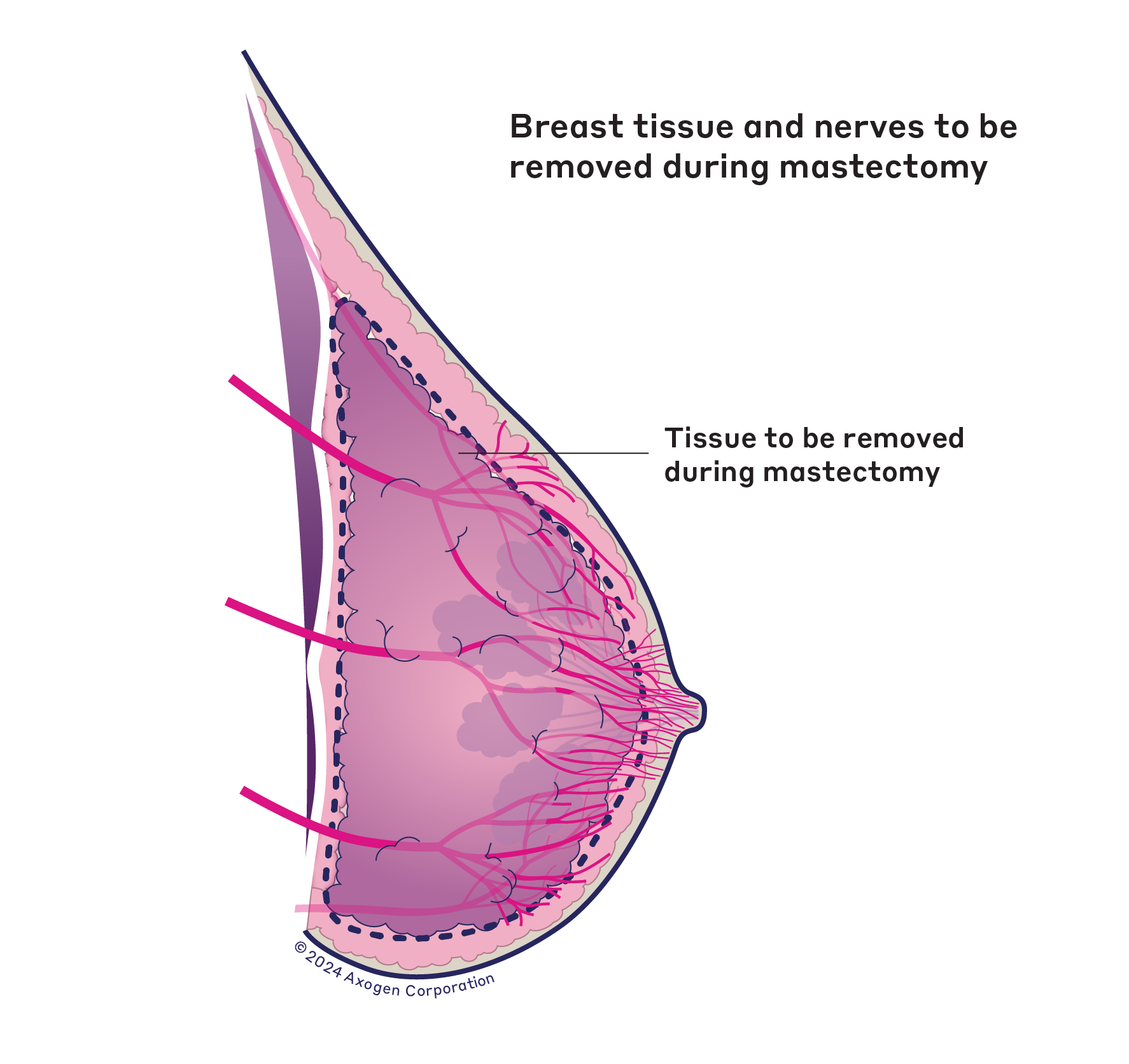
Figure 2: Breast tissue and nerves to be removed during nipple-sparing mastectomy
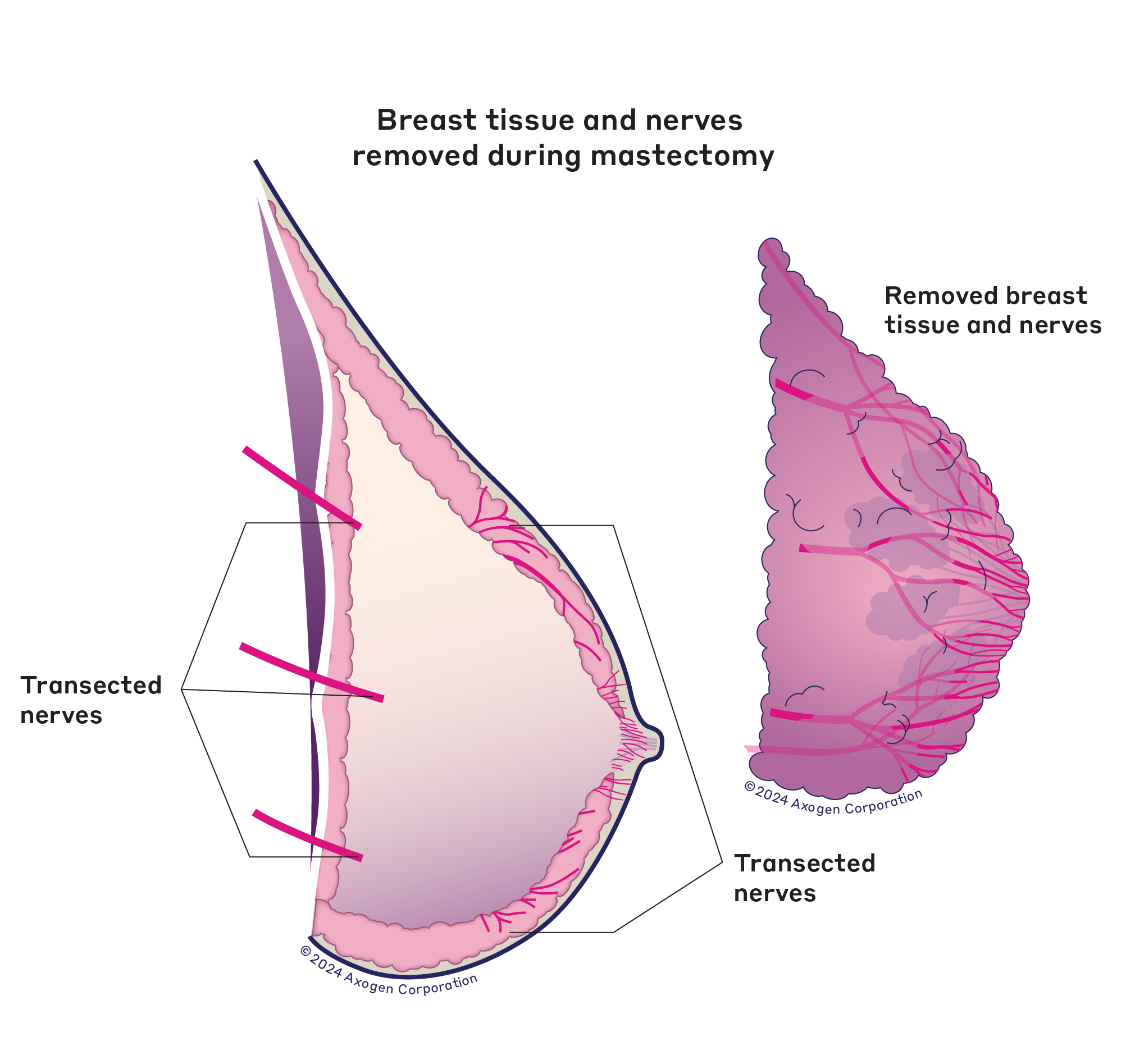
Figure 3: Breast tissue and nerves removed during nipple-sparing mastectomy
When a nerve is cut, a space or gap is created in the nerve, making it impossible to transmit sensory signals from the nipple and areola area, or much of the surrounding breast skin, similar to cutting an electrical cord on a TV.2,3 No signal means a loss of function, which may mean a loss of feeling (numbness) to your breast.
Under the right conditions, nerve fibers may regenerate to some extent on their own. However, this is highly variable, and studies show that without nerve repair, most people report significant ongoing numbness in their reconstructed breasts. People who undergo nipple-sparing mastectomy may recover slightly more sensation than those who do not, but without repair, the intercostal nerves are unlikely to regain sensation on their own—especially in an implant-based breast reconstruction.2
How will sensation loss impact my life after mastectomy?
Numbness can impact your life in many ways. It can be distressing when you can no longer feel a soft touch or the embrace of a loved one, and it can impact your self-confidence or feeling of “wholeness.”1 Research has shown that loss of breast sensation can affect body image and psychological health, too.3 For many women, breasts they cannot feel do not feel like their own.
Loss of sensation can also pose a safety hazard. You may not be able to feel cuts, rashes or burns—or even the poke of a bra wire due to the lack of protective sensation.2,3 You also might not notice everyday issues such as your seatbelt not being positioned properly or your swimsuit falling out of place. It might become uncomfortable to sleep on your stomach or side.
But this doesn’t necessarily mean you need to accept total numbness as your new normal. A surgical technique called Resensation, or breast neurotization, gives a carefully chosen nerve a chance to regenerate, which may restore some level of sensation in your reconstructed breasts.
During breast reconstruction with Resensation, the plastic surgeon uses a nerve allograft, processed donor nerve, to bridge the gap between two cut nerves in the breast. Over time, the nerve fibers regenerate, becoming a part of your own body. As the nerve fibers grow, they have the potential to gradually restore sensation to the breasts.
Read more about how Resensation works during implant breast reconstruction.
How do I talk to my doctor about sensation loss and Resensation?
Your breast surgeon and plastic surgeon can help you understand all your mastectomy and reconstruction options, including Resensation. It’s okay if you don’t know where to start. Here are a few things you might ask to get the conversation started:
- Will I have any feeling in my chest after my mastectomy?
- Do you perform Resensation? (If the answer is no, our surgeon locator can help.)
- Am I a good candidate for Resensation?
- How does nerve regeneration and recovery work?
When you’re navigating a mastectomy, it’s normal to have many questions about the procedure, including the effects of chest numbness and the potential for restoring sensation. For even more answers about mastectomy, numbness and Resensation, visit our FAQ.
References
- Crohan S, Campbell A. Breast sensation research report. Inspired Health. October 2020. Report on file at Axogen (MKTG-0302 R00).
- O’Neill RC, et al. Modern approaches to breast neurotization. Clin Plast Surg. 2023;50(2):347-355. doi:10.1016/j.cps.2022.10.003
- Coopey S, et al. Careful where you cut: strategies for successful nerve-preserving mastectomy [published correction appears in Plast Reconstr Surg Glob Open. 2024 May 28;12(5):e5943. doi: 10.1097/GOX.0000000000005943]. Plast Reconstr Surg Glob Open. 2024;12(5):e5817. Published 2024 May 15. doi:10.1097/GOX.0000000000005817
This information, including illustrations, is noncommercial, provided for educational purposes only and does not constitute medical advice or substitute for professional medical advice. The level of sensation restored following use of the Resensation technique may vary and cannot be guaranteed, due to unique anatomy and other considerations. Please consult your surgeon for more detailed information.
Some links will navigate you away from the Resensation website. Links outside of resensation.com are provided as a resource to the viewer, and do not constitute an endorsement or recommendation by Axogen. Axogen accepts no responsibility for or control over the content of the linked sites.
Resensation Articles

What happens during implant breast reconstruction with Resensation®?
By repairing sensory nerves, Resensation® enables you to potentially regain sensation to your chest. Read how this procedure works during…
Read More
how resensation® helped Leanna feel secure in her family’s future
With Resensation®, Leanna can be there to watch her kids grow up—without losing the feeling of being whole.
Read More
post-surgery sensory retraining: instructions and video guide
Sensory retraining is a series of exercises designed to help you reconnect with your body after breast reconstruction with Resensation®.
Read More
Breast self-exams: why, when and how
A breast self-exam is a useful tool for the early detection of breast cancer.
Read More